Are Your Symptoms
Affecting Your Quality Of Life?
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.

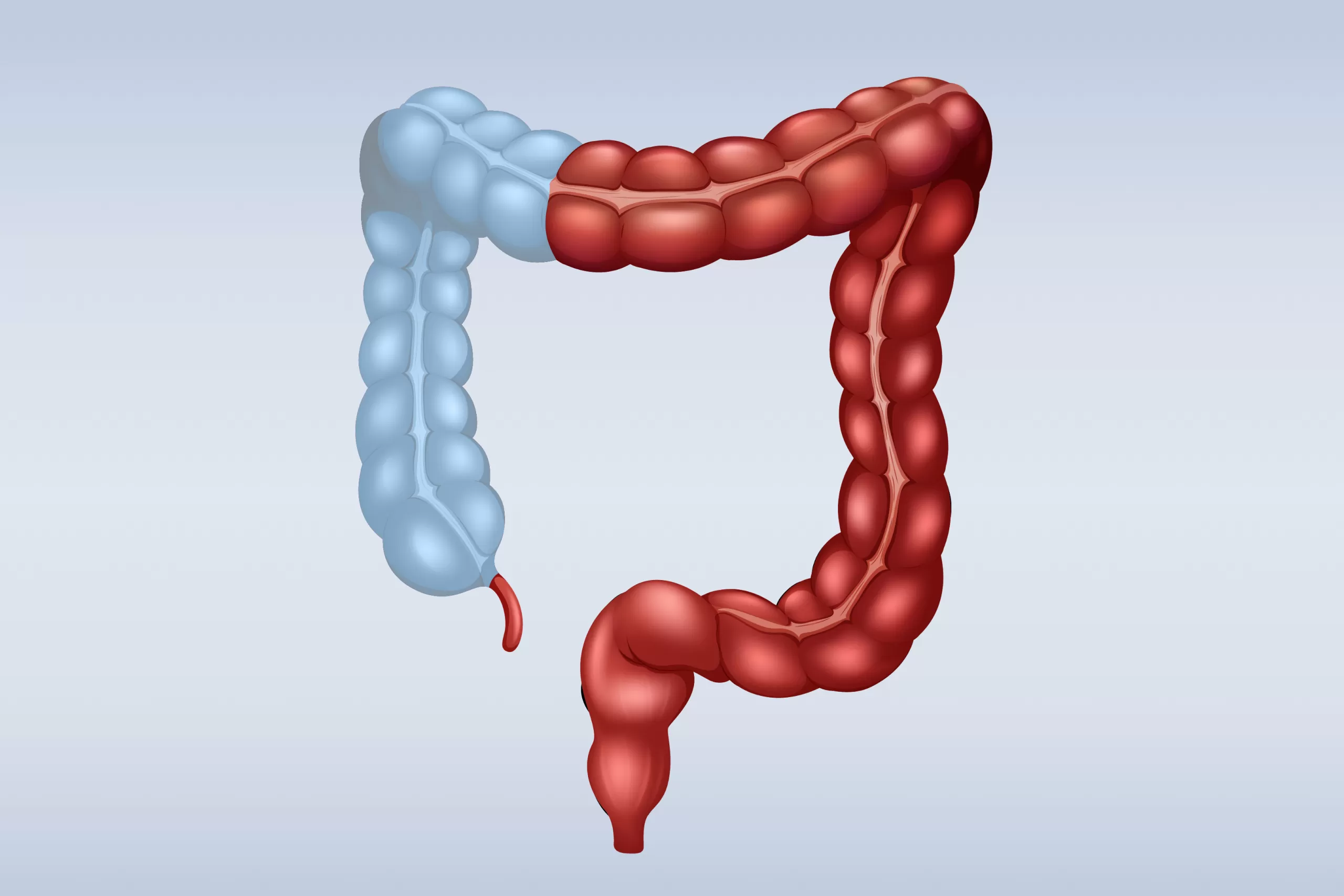
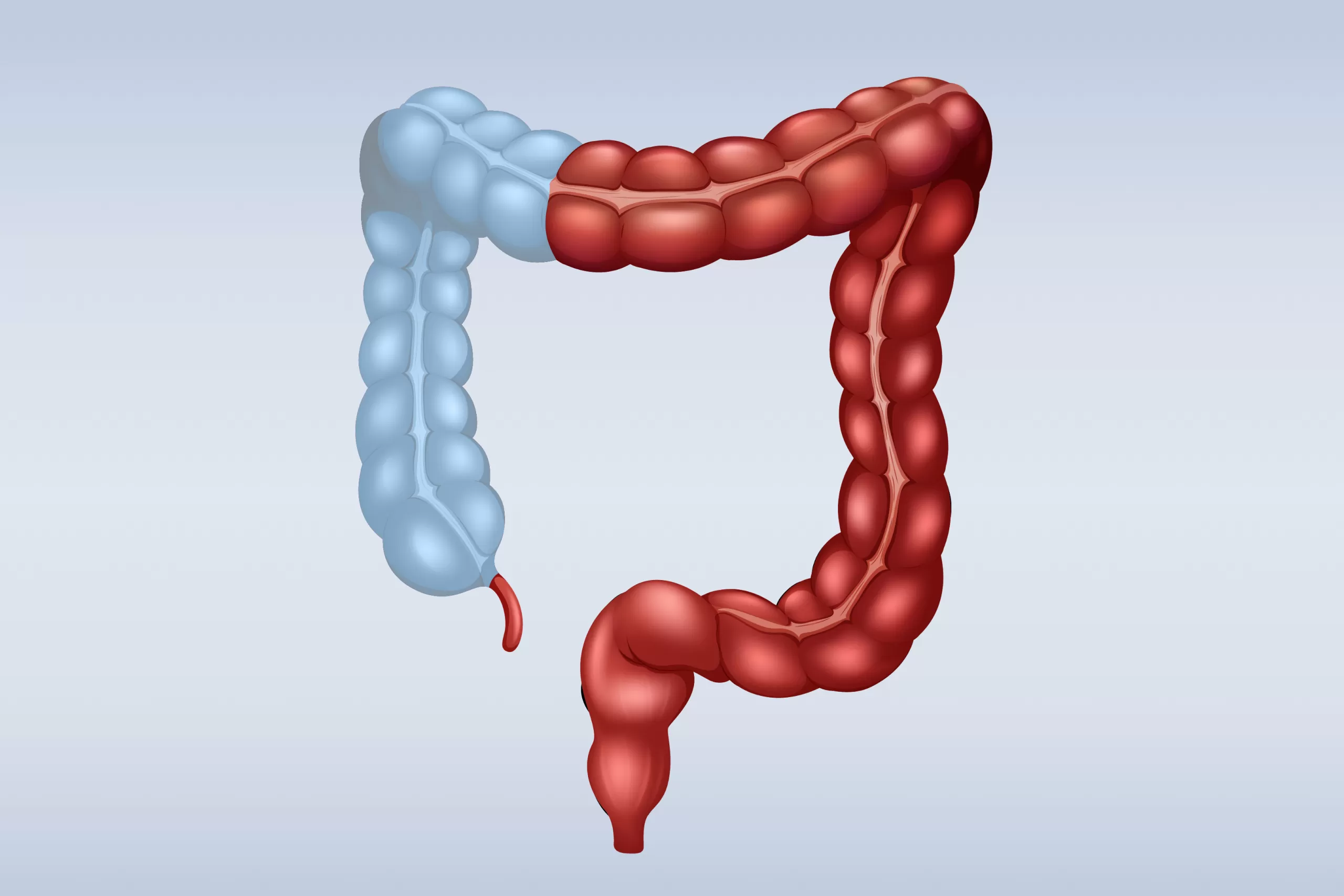

Ulcerative colitis is a chronic inflammatory condition that affects the colon and rectum, characterised by long-lasting inflammation and ulcers in the innermost lining of these organs. It is a type of inflammatory bowel disease (IBD) that causes persistent inflammation, which can result in a variety of symptoms and complications.
The disease typically alternates between flare-ups, when symptoms are active and severe, and periods of remission, when symptoms are reduced or absent.
Ulcerative colitis presents a range of symptoms primarily affecting the gastrointestinal tract. These symptoms can vary in severity. Common symptoms affecting the gastrointestinal tract include:
Diarrhoea can range from mild to severe, often with blood or mucus due to inflammation and ulceration of the colon lining.
These are common, usually felt in the lower abdomen, resulting from inflammation and ulceration of the colon, which causes muscles in the intestinal wall to contract more frequently and forcefully.
Inflammation in the rectum (proctitis) can cause pain and a sensation of incomplete evacuation. Rectal bleeding is caused by ulcers and erosions in the colon lining, which bleed and produce bright red blood in the stool.
There is often an urgent need for a bowel movement, which can be difficult to control. This is caused by the inflamed colon lining becoming more sensitive and reactive, resulting in a sudden, intense need to pass stool.
This is the persistent feeling of needing to pass stool even when the bowel is empty due to inflammation of the rectum (proctitis), which causes a sensation of incomplete evacuation and a constant urge to defecate.
Ulcerative colitis is a complex condition with an exact cause that remains unknown, but it is believed to result from a combination of genetic, immune system, and environmental factors.
Genetics: A family history of inflammatory bowel disease (IBD) significantly increases the risk, as certain genetic mutations may increase susceptibility to the disease. Individuals with close relatives, such as parents or siblings, with IBD are at a higher risk due to inherited genetic factors.
Immune System: In ulcerative colitis, the immune system mistakenly attacks the cells in the colon lining. This autoimmune reaction causes chronic inflammation, leading to the symptoms associated with the disease.
Environmental Triggers: While environmental factors such as diet, stress, and infections do not cause ulcerative colitis, they can trigger flare-ups or exacerbate existing symptoms. Certain foods, for example, can irritate the colon, stress can have an impact on immune function, and infections can cause an inflammatory response in the already sensitive colon.

Diagnosing ulcerative colitis involves tests and procedures to accurately identify the condition and distinguish it from similar conditions, such as Crohn’s disease and IBS.
This checks for anaemia and signs of inflammation. Blood tests also measure levels of inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), which can indicate active inflammation in the body.
This detects the presence of blood, infections, or inflammatory markers, which can help rule out infections caused by bacteria, viruses, or parasites that may cause similar symptoms. Stool tests can also measure calprotectin or lactoferrin, proteins that are elevated in the presence of intestinal inflammation.
A colonoscopy or sigmoidoscopy allows doctors to visually inspect the colon lining for signs of inflammation, ulcers, and bleeding. They also enable the doctor to take biopsies (small tissue samples) from the colon lining to check for disease or abnormalities.
CT scans and MRIs provide detailed images of the gastrointestinal tract. These tests can help identify the extent and severity of inflammation, as well as complications such as abscesses or strictures.
Non-surgical treatments aim to reduce inflammation, control symptoms, and maintain remission. These include:
Your doctor may prescribe different types of medication depending on the severity of the condition. These can include anti-inflammatory drugs like aminosalicylates, corticosteroids for more severe flare-ups, or immunosuppressants to control the body’s immune response. Your doctor may recommend these medications if you’re experiencing active symptoms, to help achieve remission, or as a long-term strategy to prevent future flare-ups.
When non-surgical treatments fail or complications arise, surgery may be needed. Types of surgical procedures include:
This surgery removes the entire colon and rectum. The end of the small intestine is then brought out through an opening in the belly (stoma) to allow waste to exit into an external pouch. It’s usually done when the condition is severe and other treatments haven’t worked, or if complications like severe bleeding or cancer occur.
In this procedure, the colon and rectum are removed, but the anus is preserved. A pouch is created from the end of the small intestine and connected to the anus, allowing for a more natural way of passing stool. It may be a good option for those who need surgery but want to avoid having a permanent external pouch.
This involves removing the entire colon while leaving the rectum intact. The end of the small intestine (ileum) is then connected to the rectum. This procedure is suitable for patients who have a relatively healthy rectum but require colon removal due to severe disease.
This procedure involves removing only the diseased portion of the colon and reconnecting the healthy sections. It is suitable for patients whose disease is limited to specific parts of the colon, preserving as much of the healthy colon as possible.
If you’ve had a temporary ileostomy to allow the bowel to heal, this surgery reconnects the small intestine to the rectum or anus after healing. The stoma is closed, and normal bowel function is restored, allowing you to have bowel movements through the anus again.
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.

Ulcerative colitis cannot be entirely prevented, but certain measures can help manage symptoms and reduce the risk of flare-ups.
A balanced diet rich in fruits, vegetables, and whole grains supports gut health. Avoiding foods that trigger symptoms, such as spicy or high-fat foods, and incorporating probiotics to maintain a healthy gut microbiome can also be beneficial. Stress management through meditation, exercise, or therapy can help reduce the frequency and severity of flare-ups.
Regular medical check-ups, early intervention, and adherence to prescribed treatments are recommended for managing ulcerative colitis. Additionally, avoiding smoking, staying hydrated, and maintaining a healthy weight are necessary for overall health and managing ulcerative colitis.
MBBS (S’pore)|
M.Med (Surgery)|
MRCS (Ireland)|
FRCS (Edin)|
王健名医生
Dr. Calvin Ong is a Senior Consultant with more than 15 years of surgical experience. He specializes in colorectal and general surgery, performing minimally invasive as well as advanced robotic surgeries for benign and malignant colorectal conditions, including inflammatory bowel disease, pelvic floor disorders, colorectal cancer, and hernia repair. He is dedicated to providing high-quality, personalised care for his patients.
Dr. Ong graduated with a Bachelor’s degree in medicine and surgery from the National University of Singapore in 2008 and completed his Masters of Medicine (Surgery) at the same institute. He finished his advanced specialist training in 2016 and became a fellow of the Royal College of Surgeons of Edinburgh.
For Singaporeans, Singapore Permanent Residents and Foreigners. Please speak to our friendly clinic staff about using your insurance plans.
*Extended Panel
Farrer Park Medical Centre
#14-12, 1 Farrer Park Station Road
Singapore 217562
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Alvernia Hospital
#08-62, Medical Centre D
820 Thomson Road
Singapore 574623
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Elizabeth Novena Specialist Centre
#10-48/49, 38 Irrawaddy Road
Singapore 329563
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Parkway East Hospital
#05-08, 319 Joo Chiat Place
Singapore 427989
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Gleneagles Medical Centre
6 Napier Road #06-16
Singapore 258499
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Ulcerative colitis is an inflammatory bowel disease (IBD) that causes chronic inflammation and ulcers in the colon and rectum, resulting in symptoms such as bleeding and severe abdominal pain. IBS is a functional gastrointestinal disorder without inflammation or ulcers, characterised by symptoms like cramping, abdominal pain, bloating, gas, and changes in bowel habits.
Stress, certain foods, infections, and nonsteroidal anti-inflammatory medications (NSAIDs) can all trigger flare-ups. Each individual may have different triggers, and identifying and avoiding these can help manage the condition.
With proper management, many people with ulcerative colitis can lead full and active lives. Medications, lifestyle changes, and, in some cases, surgery can help control symptoms and keep the disease in remission, reducing its impact on daily life.
Yes, complications can include severe bleeding, dehydration, bone loss, inflammation of the skin, joints, and eyes, toxic megacolon, perforated colon, and an increased risk of colon cancer. To prevent these outcomes, the disease must be managed effectively.