Are Your Symptoms
Affecting Your Quality Of Life?
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.




Pelvic floor disorders involve the weakening or injury of the muscles, ligaments, and connective tissues that support the pelvic organs, including the bladder, uterus, and rectum.
These disorders can lead to symptoms such as organ prolapse, incontinence, and pelvic pain. While they can affect both men and women, they are more common in women and can significantly impact daily activities.
This happens when the pelvic organs, like the bladder, uterus, or rectum, drop from their normal positions and push into the vaginal area because the pelvic floor muscles are weak. This can cause discomfort and a feeling of pressure.
This is when a person loses control over bowel movements, leading to accidental leakage of stool or gas. It can happen because the pelvic floor muscles are weak, nerves are damaged, or due to other health issues. There are two main types:
This occurs when the muscles that support the pelvic organs don’t work properly. It can cause symptoms like pain, difficulty controlling bowel or bladder movements, and pelvic organ prolapse. There are two types:
Pelvic floor disorders involve symptoms caused by weakened or dysfunctional pelvic floor muscles.
Pelvic floor disorders can result from various factors that weaken or damage the muscles and tissues supporting the pelvic organs.
Vaginal delivery can stretch and weaken the pelvic floor muscles, especially with multiple or complicated deliveries. The more pregnancies and deliveries a woman has, the higher the risk of developing pelvic floor disorders.
Muscle tone naturally decreases with age, increasing the likelihood that pelvic organs shift out of place. This makes it harder for the pelvic floor to support the bladder, bowel, and reproductive organs, leading to disorders such as incontinence and pelvic organ prolapse.
Constipation or heavy lifting puts repeated pressure on the pelvic floor. Over time, this repeated pressure can stretch and weaken the muscles, resulting in urinary and faecal incontinence or pelvic organ prolapse.
Obesity and chronic respiratory disorders that cause persistent coughing can lead to pelvic floor disorders. Obesity adds extra weight and pressure on the pelvic floor, while chronic coughing can directly weaken or damage the pelvic muscles and nerves.
As estrogen and progesterone levels decrease during menopause, the pelvic floor muscles may become weaker and less elastic.

Diagnosing pelvic floor disorders involves several steps to accurately identify the condition and determine the best treatment approach.
Discussing a patient’s symptoms, health history, and past surgeries or pregnancies helps the doctor evaluate the nature and severity of the disorder. This also reveals potential causes of pelvic floor weakness or dysfunction.
A thorough examination of the pelvic muscles and organs, including a pelvic exam, is necessary to check for signs of prolapse, muscle weakness, or other abnormalities.
Ultrasounds, MRIs, or CT scans are used to visualise the pelvic structures and assess abnormalities. These tests provide detailed images of the pelvic organs, muscles, and tissues, helping to pinpoint the location and severity of the disorder.
This test assesses bladder function by measuring urine pressure and flow. It can diagnose urinary incontinence and other bladder issues related to pelvic floor disorders.
This X-ray or MRI test evaluates how well the rectum empties stool, making it useful for diagnosing conditions like rectal prolapse or other bowel movement disorders linked to pelvic floor dysfunction.
This test assesses the function of the nerves in the pelvic area and helps identify any nerve damage contributing to pelvic floor disorders. Nerve function tests can include electromyography (EMG), which measures the electrical activity of muscles and nerves.
Non-surgical treatments aim to strengthen the pelvic muscles, alleviate symptoms, and address specific issues without the need for surgery.
Medication for pelvic floor disorders can manage symptoms through various types of drugs. Muscle relaxants relieve pelvic muscle spasms and pain; topical oestrogen helps to strengthen pelvic tissues, particularly in postmenopausal women; and bladder control medications reduce urinary urgency and frequency associated with an overactive bladder.
When non-surgical treatments fail or complications arise, surgery may be required. The main surgical treatment options for pelvic floor disorders are:
This procedure corrects rectal prolapse, where the rectum protrudes through the anus, by repositioning the rectum and attaching it to the sacrum to hold it in place. It addresses symptoms such as rectal bulging, discomfort, and incontinence, while restoring normal rectal anatomy and function. A colorectal surgeon ensures the rectum is properly repositioned and secured to prevent recurrence.
This procedure repairs defects or damage in the perineum (the area between the vagina and anus). It involves suturing torn muscles and tissues to restore normal function and support. It is often performed after childbirth or trauma that has caused damage to the perineal area. Perineal repair restores the integrity of the pelvic floor muscles and alleviates symptoms such as incontinence and pain. A colorectal surgeon ensures that the damaged tissues are properly sutured and the pelvic floor is adequately supported to restore function.
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.
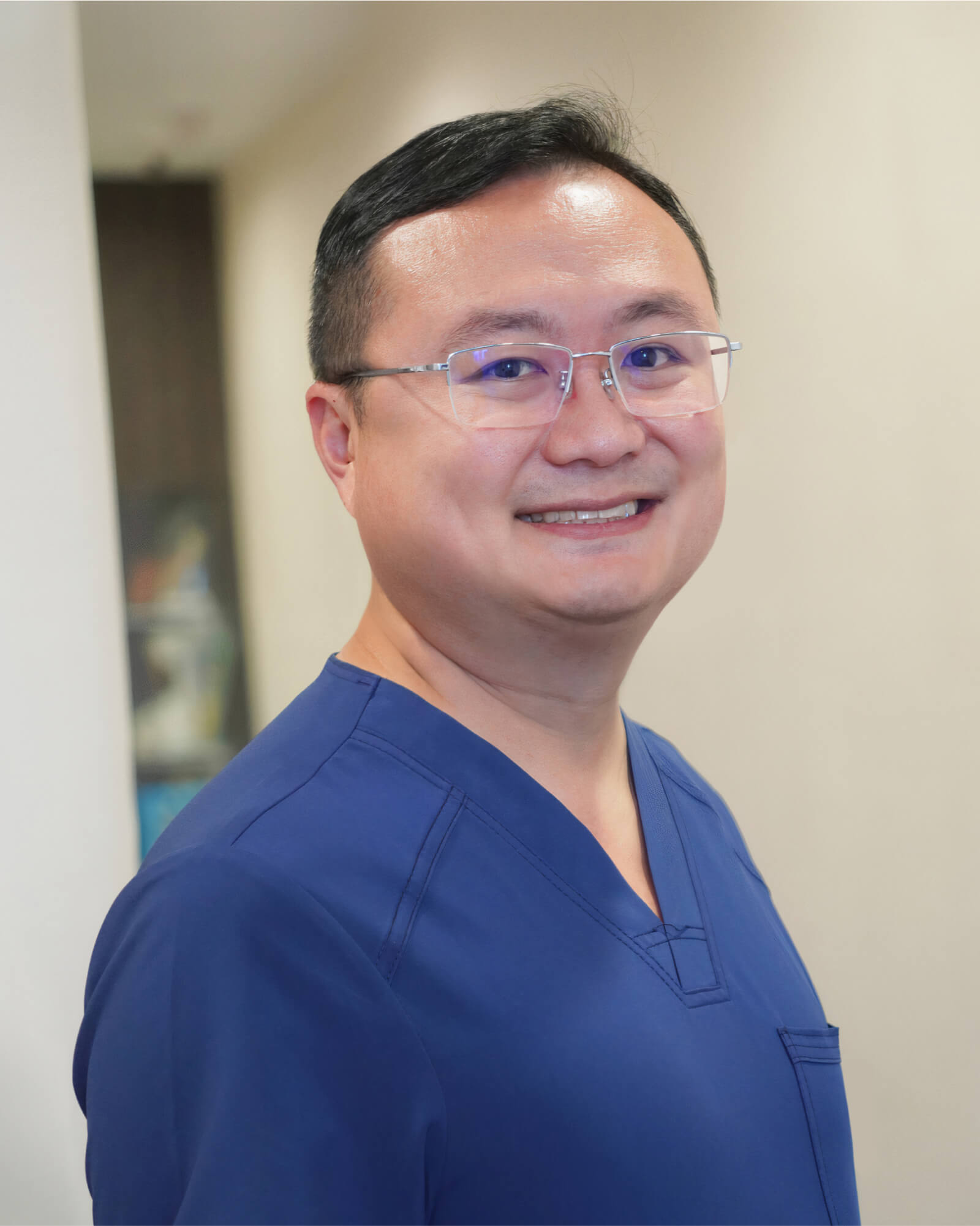
MBBS (S’pore)|
M.Med (Surgery)|
MRCS (Ireland)|
FRCS (Edin)|
王健名医生
Dr. Calvin Ong is a Senior Consultant with more than 15 years of surgical experience. He specializes in colorectal and general surgery, performing minimally invasive as well as advanced robotic surgeries for benign and malignant colorectal conditions, including inflammatory bowel disease, pelvic floor disorders, colorectal cancer, and hernia repair. He is dedicated to providing high-quality, personalised care for his patients.
Dr. Ong graduated with a Bachelor’s degree in medicine and surgery from the National University of Singapore in 2008 and completed his Masters of Medicine (Surgery) at the same institute. He finished his advanced specialist training in 2016 and became a fellow of the Royal College of Surgeons of Edinburgh.
For Singaporeans, Singapore Permanent Residents and Foreigners. Please speak to our friendly clinic staff about using your insurance plans.
*Extended Panel
Farrer Park Medical Centre
#14-12, 1 Farrer Park Station Road
Singapore 217562
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Alvernia Hospital
#08-62, Medical Centre D
820 Thomson Road
Singapore 574623
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Elizabeth Novena Specialist Centre
#10-48/49, 38 Irrawaddy Road
Singapore 329563
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Parkway East Hospital
#05-08, 319 Joo Chiat Place
Singapore 427989
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Gleneagles Medical Centre
6 Napier Road #06-16
Singapore 258499
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Yes, men can develop pelvic floor disorders. While it is more common in women, men can suffer from conditions like urinary incontinence, faecal incontinence, and chronic pelvic pain due to factors such as prostate surgery, chronic constipation, or nerve damage.
If a pelvic floor disorder is left untreated, the condition can progressively worsen over time, leading to an increased risk in complications and increased severity of symptoms. Here are some potential complications that may develop:
Recovery time varies depending on the type of surgery and individual patient factors. Generally, full recovery may take several weeks. Adhering to post-surgical care instructions, avoiding heavy lifting, and gradually resuming normal activities are necessary. Your surgeon will provide specific guidance tailored for your recovery and overall health.