Are Your Symptoms
Affecting Your Quality Of Life?
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.

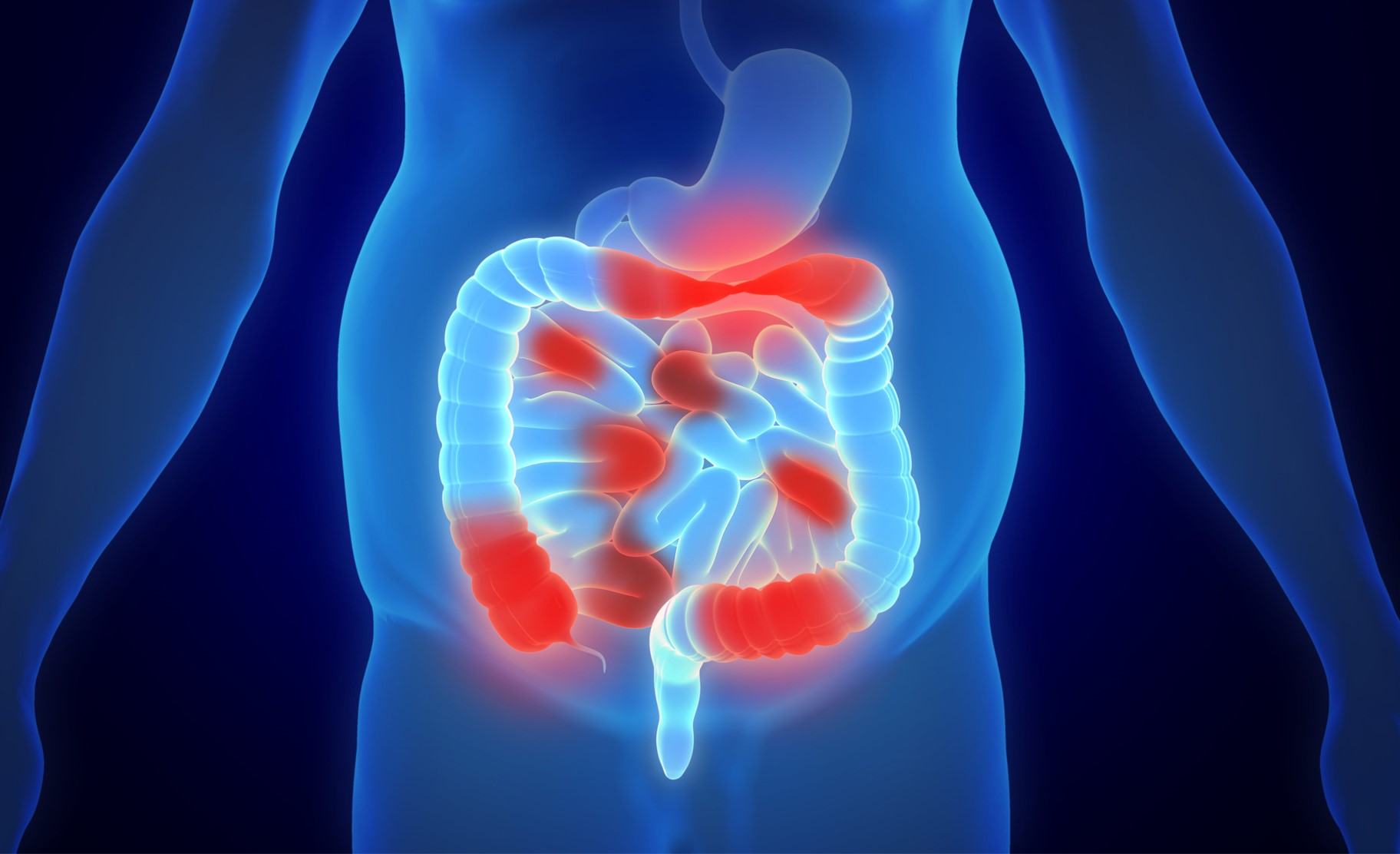

Crohn’s disease is a chronic inflammatory condition that affects the digestive tract, which extends from the mouth to the anus, commonly targeting the small intestine and the beginning of the colon.
As a type of inflammatory bowel disease (IBD), it results in long-term inflammation that can damage the digestive system. The disease typically alternates between periods of flare-ups, when symptoms are active and more severe, and periods of remission, when symptoms are reduced or absent.
Crohn’s disease presents a wide range of symptoms primarily affecting the gastrointestinal tract, as well as systemic and extraintestinal manifestations. These symptoms can vary in severity. Common gastrointestinal related symptoms include:
This can range from mild to severe and may contain mucus or blood, indicating the level of inflammation in the intestines. The inflammation disrupts the normal absorption of water in the intestines, resulting in loose stools.
Intestinal inflammation can cause significant pain and cramping, most commonly felt in the lower right abdomen but can occur elsewhere. This pain occurs when the intestines contract to move food, which can be painful when the intestinal walls are inflamed.
When inflammation in the intestines leads to the formation of ulcers, these ulcers can bleed. Depending on where the bleeding occurs in the intestine, this can result in bright red blood or darker stools.
Ulcers in the mouth, similar to canker sores, can develop due to the inflammation caused by Crohn’s disease. These sores are a result of the body’s general inflammatory response.
Chronic inflammation and pain in the intestines can reduce appetite and impair nutrient absorption, leading to unintended weight loss.
Crohn’s disease is believed to be caused by a combination of factors, which may increase the risk of developing the disease.
Age and Genetics: Crohn’s disease is typically diagnosed in young adults aged 15 to 35, but it can occur at any age. Having a family history of Crohn’s disease or a first-degree relative with the condition significantly increases risk, suggesting a strong genetic component.
Immune System: Crohn’s disease is believed to involve an abnormal immune response that mistakenly attacks the digestive tract, leading to chronic inflammation and damage to the intestines.
Smoking: Smoking increases the risk of developing Crohn’s disease, exacerbates its severity, and increases the risk of recurrence following treatment. Quitting smoking can help improve prognosis and reduce the frequency of flare-ups.

Several tests and procedures are used to diagnose Crohn’s disease and distinguish it from conditions with similar symptoms, such as ulcerative colitis and irritable bowel syndrome.
Used to check for anaemia and signs of inflammation. These results provide information about the presence of Crohn’s disease and the extent of inflammation.
Used to detect blood or infections. Blood in the stool may indicate bleeding in the digestive tract, a common symptom of Crohn’s disease. It can also rule out infections that may cause similar symptoms, such as diarrhoea or abdominal pain.
These procedures involve inserting a thin, flexible tube with a camera into the rectum, allowing doctors to visually inspect inflammation, ulcers, and other abnormalities in the colon and rectum. Small tissue samples (biopsies) may be collected for further examination to confirm the diagnosis of Crohn’s disease.
Capsule endoscopy involves swallowing a small capsule containing a camera. The capsule travels through the digestive tract and captures images of the small intestine. This test is useful for examining parts of the small intestine that are difficult to access using traditional endoscopy, helping identify areas of inflammation, bleeding, and other abnormalities indicative of Crohn’s disease.
CT scans and MRIs provide detailed images of the gastrointestinal tract, helping to identify inflammation, strictures (narrowing), and fistulas (abnormal connections) in the intestines. These non-invasive imaging techniques offer comprehensive views that assess the extent and severity of Crohn’s disease.
Treating Crohn’s disease often involves medications to reduce inflammation, manage symptoms, and maintain remission.
Surgical treatment is considered for Crohn’s disease when medications fail to manage symptoms or complications arise.
A bowel resection involves removing the diseased portion of the intestine and connecting the healthy sections (anastomosis).This procedure is typically required for patients with severe, localised Crohn’s disease that has not responded to medical therapy or has led to complications such as obstructions or perforations.
Strictureplasty is used to treat narrowed sections of the intestine, known as strictures. This procedure widens the affected area without removing any part of the intestine. This procedure is typically indicated for patients with multiple or long segments of strictures, especially when preserving bowel length is crucial to avoid short bowel syndrome.
Fistulas are abnormal connections between the perianal region and the anal canal. Anal fistulas are common in Crohn’s disease and treatment involves fistulotomies, setons and sometimes even flap repairs.
Proctocolectomy involves removing the rectum and part of the colon, often followed by creating a stoma, which is an opening in the abdominal wall to allow waste to exit the body. This procedure is considered for severe cases of Crohn’s disease where other treatments have failed and the colon and rectum are extensively damaged.
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.

Preventing Crohn’s disease is challenging due to its complex causes, but certain measures may help reduce the risk. Maintaining a healthy diet rich in fruits, vegetables, whole grains, and lean proteins supports digestive health. Stress management through relaxation techniques is also beneficial to overall digestive health. Avoiding NSAIDs that can irritate the digestive tract and limiting antibiotic use can help to manage potential risks. Cessation of smoking can also greatly improve the condition. Additionally, regular check-ups and monitoring infections are recommended.
While complete prevention may not be possible, these measures can improve overall well-being and potentially delay the onset of Crohn’s disease.
MBBS (S’pore)|
M.Med (Surgery)|
MRCS (Ireland)|
FRCS (Edin)|
王健名医生
Dr. Calvin Ong is a Senior Consultant with more than 15 years of surgical experience. He specializes in colorectal and general surgery, performing minimally invasive as well as advanced robotic surgeries for benign and malignant colorectal conditions, including inflammatory bowel disease, pelvic floor disorders, colorectal cancer, and hernia repair. He is dedicated to providing high-quality, personalised care for his patients.
Dr. Ong graduated with a Bachelor’s degree in medicine and surgery from the National University of Singapore in 2008 and completed his Masters of Medicine (Surgery) at the same institute. He finished his advanced specialist training in 2016 and became a fellow of the Royal College of Surgeons of Edinburgh.
For Singaporeans, Singapore Permanent Residents and Foreigners. Please speak to our friendly clinic staff about using your insurance plans.
*Extended Panel
Farrer Park Medical Centre
#14-12, 1 Farrer Park Station Road
Singapore 217562
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Alvernia Hospital
#08-62, Medical Centre D
820 Thomson Road
Singapore 574623
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Elizabeth Novena Specialist Centre
#10-48/49, 38 Irrawaddy Road
Singapore 329563
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Parkway East Hospital
#05-08, 319 Joo Chiat Place
Singapore 427989
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Gleneagles Medical Centre
6 Napier Road #06-16
Singapore 258499
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Crohn’s disease and ulcerative colitis are both inflammatory bowel diseases, but they differ significantly. Crohn’s disease can affect any part of the gastrointestinal tract, from the mouth to the anus, often in patches, and affects all layers of the intestinal wall. Ulcerative colitis, on the other hand, is limited to the colon and rectum, affecting only the innermost lining of the bowel.
Children and adolescents with Crohn’s disease may experience delayed growth and puberty due to malnutrition and chronic inflammation. To manage the disease and promote healthy growth and development, young patients must receive proper nutritional support as well as medical care.
Yes, people with Crohn’s disease can travel, but it requires some planning. They must carry enough medication, have a plan for managing symptoms while away from home, and be aware of healthcare facilities at the travel destination. Consult a doctor before travelling to address any concerns and ensure a smooth trip.