Are Your Symptoms
Affecting Your Quality Of Life?
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.




Inflammatory Bowel Disease (IBD) is a term used to describe chronic conditions that cause inflammation of the gastrointestinal (GI) tract, primarily Crohn’s disease and ulcerative colitis.
Crohn’s disease can affect any part of the GI tract, from the mouth to the anus, while ulcerative colitis is limited to the colon and rectum. Both conditions can cause discomfort and may lead to serious complications if not properly managed.
IBD primarily includes two types: Crohn’s disease and ulcerative colitis, each with distinct characteristics and affected areas of the GI tract.
Can affect any part of the GI tract, from the mouth to the anus. It often involves the deeper layers of the bowel wall and can cause a variety of symptoms depending on the affected area. Crohn’s disease can lead to complications such as strictures (narrowing of the bowel), fistulas (abnormal connections between different parts of the bowel), and abscesses (collections of pus).
Limited to the colon and rectum. It primarily affects the innermost lining of the colon, causing continuous inflammation and ulcers. Ulcerative colitis can lead to complications such as severe bleeding, perforated colon, and an increased risk of colon cancer.
The symptoms of IBD can vary depending on the severity and location of the inflammation. Common symptoms include:
The exact cause of IBD is unknown, but several factors are thought to contribute to its development.
Family history of IBD increases the risk. Certain genetic mutations have been associated with a higher risk of developing IBD.
An abnormal immune response that attacks the cells of the digestive tract can lead to chronic inflammation.
Certain lifestyle and environmental factors, such as smoking, diet, and stress, may influence the risk. Urban living and exposure to industrial pollutants have also been linked to higher rates of IBD.
Imbalances in the gut microbiome, including reduced diversity of gut bacteria, are often observed in patients with IBD.
IBD can occur at any age but it is most commonly diagnosed in adolescents and young adults. Males are slightly more likely to be affected in childhood than females in adulthood.

IBD is diagnosed through a variety of diagnostic procedures, including:
This checks for anaemia and inflammation markers (e.g., C-reactive protein) and other signs of inflammation.
This detects blood, pathogens, and inflammatory markers (e.g., calprotectin).
These procedures allow doctors to view the colon and rectum and take biopsies.
This procedure may be used to examine the upper GI tract, especially in Crohn’s disease.
These provide detailed images of the GI tract, allowing doctors to assess the severity of inflammation and identify complications (e.g., fistulas, abscesses).
This procedure involves swallowing a small capsule containing a camera to obtain images of the small intestine, which is especially useful for Crohn’s disease.
While there is no cure for IBD, a variety of treatments can help manage symptoms and keep the condition in remission. Treatment options include both non-surgical and surgical approaches.
Non-surgical treatments aim to manage inflammation and alleviate symptoms using various medications without the need for invasive procedures. These include:
Surgical treatments are considered when non-surgical methods fail to control symptoms or when complications arise. These include:
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.

Certain measures can help reduce the risk of flare-ups and manage IBD.
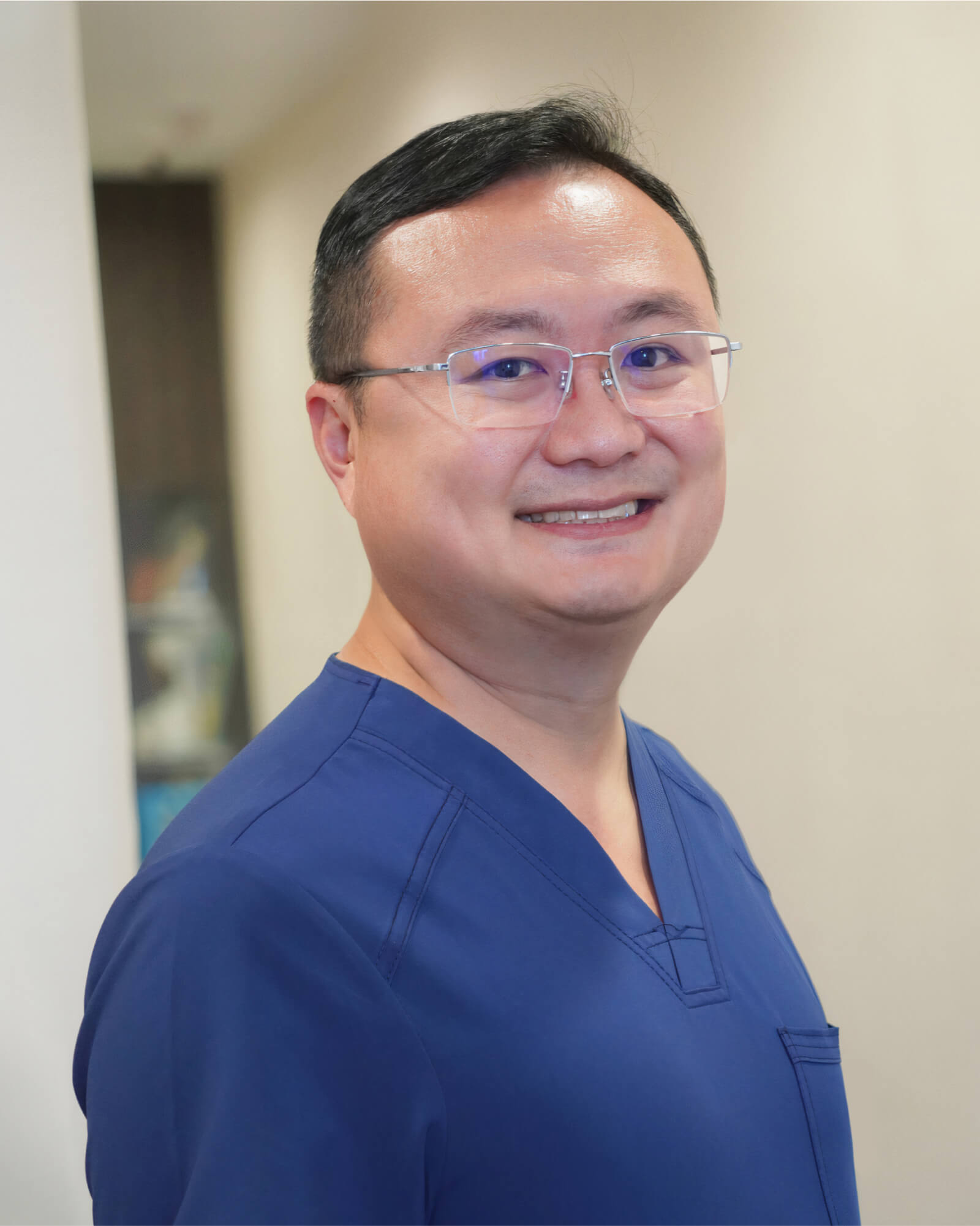
MBBS (S’pore)|
M.Med (Surgery)|
MRCS (Ireland)|
FRCS (Edin)|
王健名医生
Dr. Calvin Ong is a Senior Consultant with more than 15 years of surgical experience. He specializes in colorectal and general surgery, performing minimally invasive as well as advanced robotic surgeries for benign and malignant colorectal conditions, including inflammatory bowel disease, pelvic floor disorders, colorectal cancer, and hernia repair. He is dedicated to providing high-quality, personalised care for his patients.
Dr. Ong graduated with a Bachelor’s degree in medicine and surgery from the National University of Singapore in 2008 and completed his Masters of Medicine (Surgery) at the same institute. He finished his advanced specialist training in 2016 and became a fellow of the Royal College of Surgeons of Edinburgh.
For Singaporeans, Singapore Permanent Residents and Foreigners. Please speak to our friendly clinic staff about using your insurance plans.
*Extended Panel
Farrer Park Medical Centre
#14-12, 1 Farrer Park Station Road
Singapore 217562
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Alvernia Hospital
#08-62, Medical Centre D
820 Thomson Road
Singapore 574623
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Elizabeth Novena Specialist Centre
#10-48/49, 38 Irrawaddy Road
Singapore 329563
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Parkway East Hospital
#05-08, 319 Joo Chiat Place
Singapore 427989
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Gleneagles Medical Centre
6 Napier Road #06-16
Singapore 258499
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Untreated IBD can lead to serious complications such as strictures, fistulas, abscesses, malnutrition, and an increased risk of colorectal cancer.
The long-term outlook varies; with proper management, many people lead active, healthy lives. Continuous monitoring and treatment adjustments can manage flare-ups and maintain remission.
IBD (Inflammatory Bowel Disease) involves chronic inflammation of the GI tract and can cause severe damage, whereas IBS (Irritable Bowel Syndrome) is a functional disorder without inflammation or damage to the intestines.