Are Your Symptoms
Affecting Your Quality Of Life?
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.



Gastroscopy is a medical procedure used to examine the lining of the upper gastrointestinal tract, including the oesophagus, stomach, and duodenum (the first section of the small intestine).
It involves using a gastroscope, a long, flexible tube with a light and camera, gently inserted through the mouth and guided down the throat into the stomach and duodenum. The camera transmits images to a monitor, allowing the doctor to inspect these areas for abnormalities such as inflammation, ulcers, or tumours and sometimes to perform treatments.
Gastroscopy is used for both diagnostic and therapeutic purposes.
Diagnostic indications involve using gastroscopy to identify the cause of gastrointestinal symptoms and conditions, aiding in the diagnosis of various esophageal, stomach, and duodenal issues.
Therapeutic indications involve using gastroscopy to treat specific conditions or manage complications within the gastrointestinal tract.

Proper preparation is necessary to ensure accurate results. The preparation process typically includes:
Patients must usually fast for at least 6 to 8 hours before the procedure, avoiding all food and drink, including water, to ensure an empty stomach and clear for examination.
Certain medications may need to be adjusted or temporarily discontinued, especially blood thinners, which may raise the risk of bleeding during the procedure. Patients should consult their doctor about any current medications.
Inform the medical team of any known allergies, especially to medications or anaesthetics, as these will influence the choice of sedatives or anaesthetic agents used during the procedure.
A thorough review of the patient’s medical history, including past surgeries, chronic conditions, or recent illnesses, allows the doctor to anticipate and manage potential complications.
Arrive at the hospital or clinic at the scheduled time for pre-procedure preparations, including paperwork and initial assessments. Make arrangements for transportation home due to the sedative effects.
The gastroscopy procedure follows these steps for a thorough and safe examination:

Proper care after a gastroscopy ensures a smooth recovery.
Patients are monitored in a recovery area after the procedure until the sedative wears off. Mild throat soreness or discomfort is common and can be eased with throat lozenges or warm saline gargles. Start with small sips of water and gradually resume a normal diet, avoiding hot or spicy foods initially.
Resting for the remainder of the day is advised due to lingering sedation effects. Avoid driving or operating heavy machinery. Normal activities can usually be resumed the next day, but avoid strenuous activities for at least 24 hours. Drink plenty of fluids to help flush out the sedative and stay hydrated, which promotes a quicker recovery.
The doctor will review the gastroscopy results with the patient, either immediately after the procedure or at a follow-up appointment. Biopsy results typically take a few days to a week. The doctor will contact the patient with findings and recommendations for further treatment or additional tests if necessary.
Consult our MOH-accredited specialist for an accurate diagnosis & personalised treatment plan today.
While gastroscopy is generally considered a safe procedure, it carries some risks and potential complications. Understanding these risks helps in making informed decisions and recognising when to seek medical attention.
Common risks are typically mild and resolve quickly without requiring medical intervention, such as:
Complications from gastroscopy are rare, but patients must be aware of potential risks and know when to seek help. Seek medical attention if you experience:
The doctor will discuss initial findings with the patient after the procedure. Visual inspection during the gastroscopy may reveal conditions such as inflammation, ulcers, tumours, or other abnormalities. If a biopsy was performed, tissue samples are sent to a laboratory for analysis. Biopsy results, which take a few days to a week, provide detailed information on infections, malignancies, or other cellular abnormalities.
The doctor will review both the visual findings and biopsy results, either immediately after the procedure or at a follow-up appointment. Based on the results, a treatment plan may be recommended, including medications, lifestyle changes, further tests, or additional procedures. For example, if Helicobacter pylori infection is detected, antibiotic therapy may be prescribed. Conditions like Barrett’s oesophagus or certain ulcers may require regular monitoring with repeat gastroscopies to assess treatment effectiveness and check for progression.
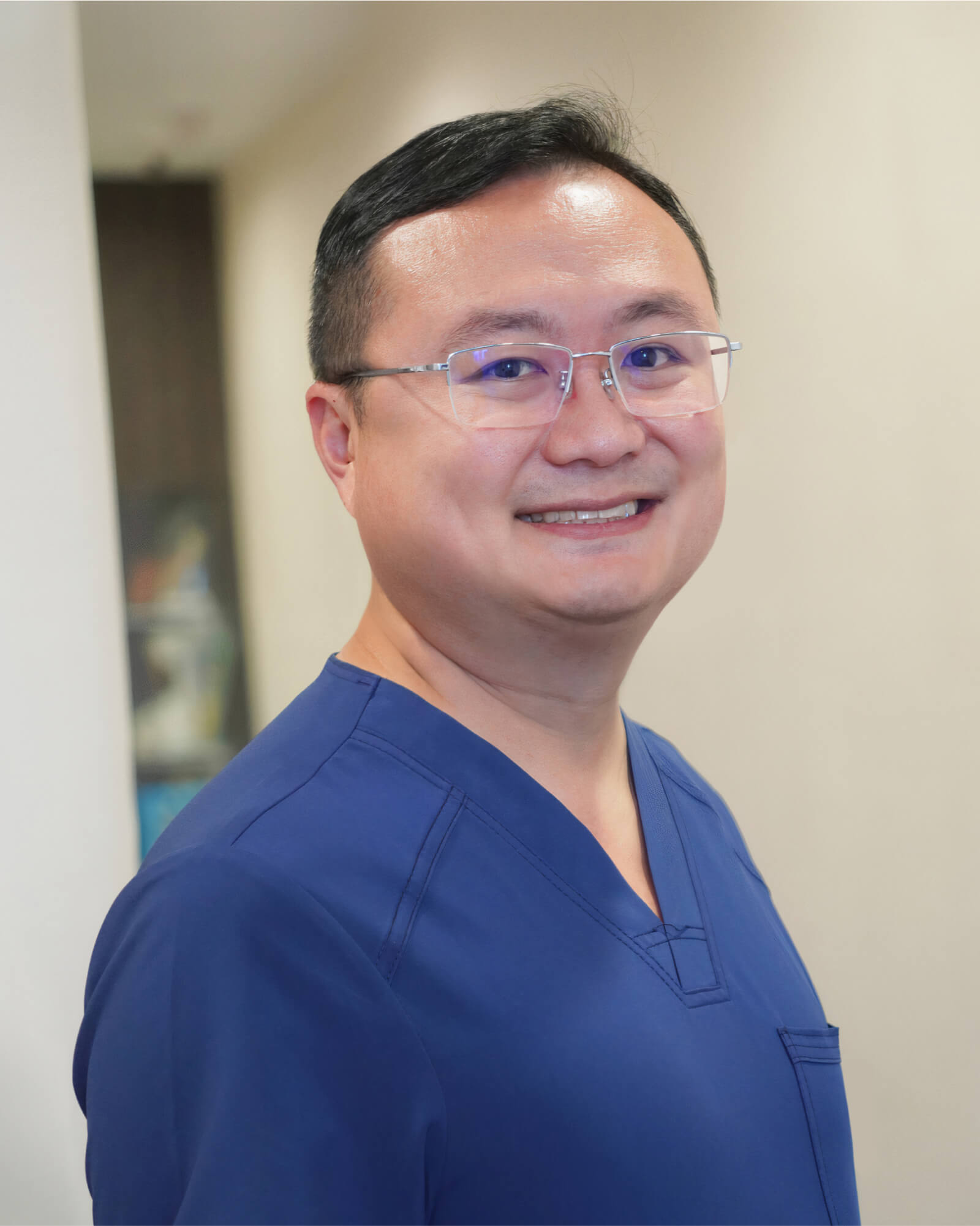
MBBS (S’pore)|
M.Med (Surgery)|
MRCS (Ireland)|
FRCS (Edin)|
王健名医生
Dr. Calvin Ong is a Senior Consultant with more than 15 years of surgical experience. He specializes in colorectal and general surgery, performing minimally invasive as well as advanced robotic surgeries for benign and malignant colorectal conditions, including inflammatory bowel disease, pelvic floor disorders, colorectal cancer, and hernia repair. He is dedicated to providing high-quality, personalised care for his patients.
Dr. Ong graduated with a Bachelor’s degree in medicine and surgery from the National University of Singapore in 2008 and completed his Masters of Medicine (Surgery) at the same institute. He finished his advanced specialist training in 2016 and became a fellow of the Royal College of Surgeons of Edinburgh.
For Singaporeans, Singapore Permanent Residents and Foreigners. Please speak to our friendly clinic staff about using your insurance plans.
*Extended Panel
Farrer Park Medical Centre
#14-12, 1 Farrer Park Station Road
Singapore 217562
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Alvernia Hospital
#08-62, Medical Centre D
820 Thomson Road
Singapore 574623
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Mount Elizabeth Novena Specialist Centre
#10-48/49, 38 Irrawaddy Road
Singapore 329563
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Parkway East Hospital
#05-08, 319 Joo Chiat Place
Singapore 427989
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments
Gleneagles Medical Centre
6 Napier Road #06-16
Singapore 258499
Appointment : (65) 6643 9922
Urgent Care : (65) 8181 2311
Monday to Friday : 9AM – 6PM
Saturday : 9AM – 1PM
Sunday & Public Holidays : By Appointments